Preterm Care
Preterm birth refers to babies born alive before 37 weeks of pregnancy are completed. These early arrivals face unique challenges, and providing appropriate care
Categories of Preterm Birth:
Extremely preterm: Babies born before 28 weeks of gestation.
Very preterm: Babies born between 28 and less than 32 weeks.
Moderate to late preterm: Babies born between 32 and 37 weeks.
Global Impact:
Approximately 13.4 million babies were born preterm in 2020 worldwide.
Preterm birth complications are the leading cause of death among children under 5 years of age, responsible for around 900,000 deaths in 2019.
Three-quarters of these deaths could be prevented with current, cost-effective interventions.
Survival Disparities:
In low-income settings, half of babies born at or below 32 weeks (2 months early) die due to a lack of feasible, cost-effective care.
In contrast, in high-income countries, almost all extremely preterm babies survive.
Suboptimal use of technology in middle-income settings contributes to an increased burden of disability among preterm survivors.
Causes of Preterm Birth:
Spontaneous preterm labor: Most preterm births occur spontaneously.
Medical reasons: Some are due to infections, other pregnancy complications, or medical indications for early induction of labor or caesarean birth.
Genetic influence: In some cases, no specific cause is identified.
Where and When Preterm Birth Occurs:
The majority of preterm births happen in southern Asia and sub-Saharan Africa.
Dramatic survival differences: Over 90% of extremely preterm babies born in low-income countries die within the first few days, while less than 10% die in high-income settings.
Preventing Preterm Birth:
Healthy pregnancy care is essential.
Key interventions include:
Counseling on healthy diet, optimal nutrition, and avoiding tobacco and substance use.
Fetal measurements, including early ultrasound to determine gestational age and detect multiple pregnancies.
Regular antenatal visits (at least 8) to identify and manage risk factors such as infections
Preterm Survivals
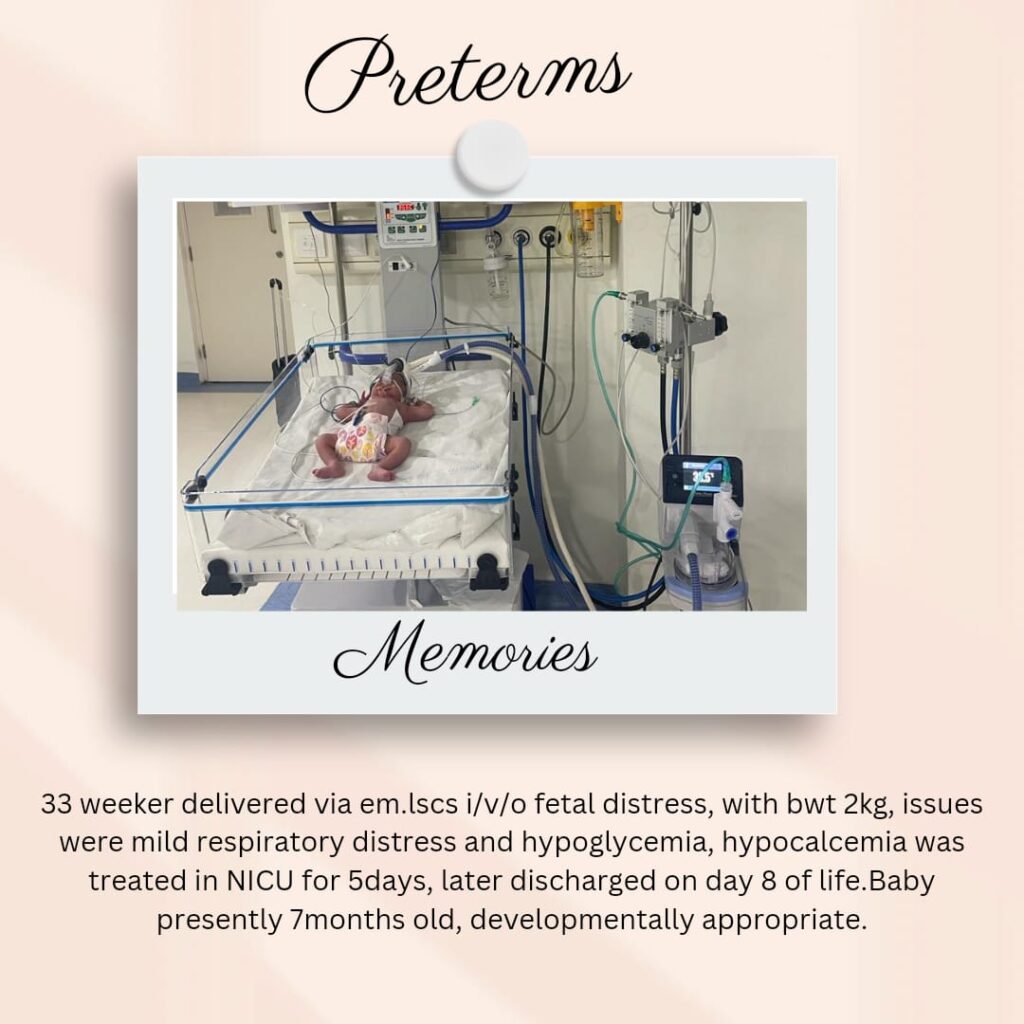
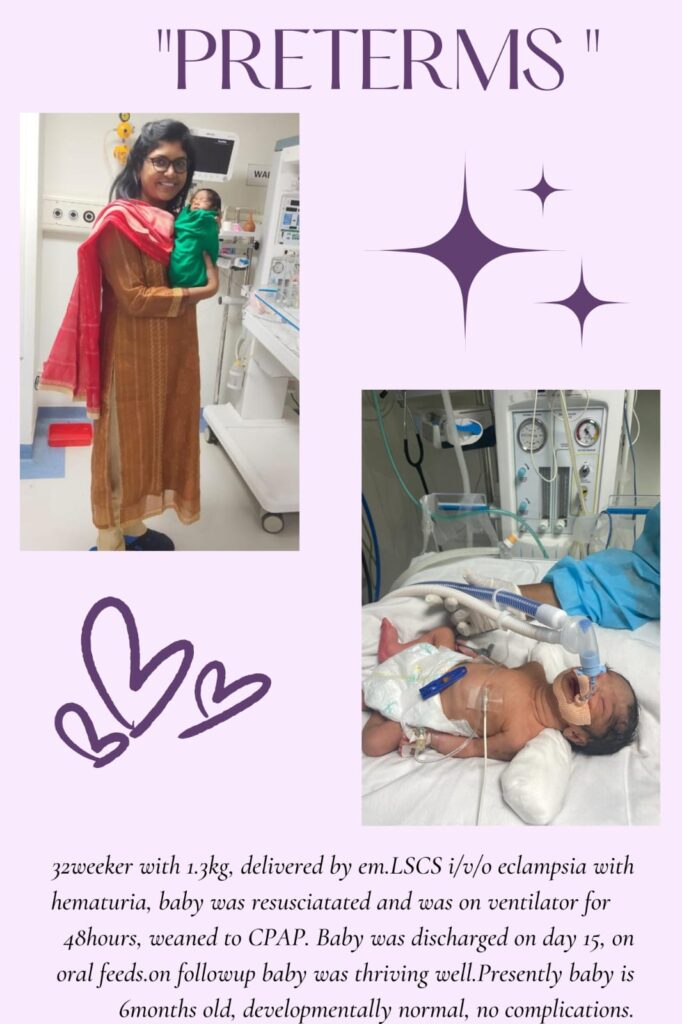
NICU Treatment

Preterm infants require specialized care in the Neonatal Intensive Care Unit (NICU) to support their unique needs.
Here are some key aspects of preterm care:
Temperature Regulation: Preterm babies struggle to maintain body temperature. NICUs provide specialized equipment to keep them warm, including incubators that create a controlled environment. These incubators help maintain the right temperature for their delicate bodies.
Breathing Support: Some preterm infants need assistance with breathing. NICUs have ventilators and other respiratory support devices to ensure proper oxygenation and lung function.
Feeding: Preterm babies may not be able to feed directly from the breast or bottle initially. NICU staff monitor their nutritional needs and provide specialized feeding methods, such as tube feeding or intravenous nutrition.
Monitoring and Observation: NICU staff closely monitor preterm infants for any signs of distress, infection, or other health issues. They assess vital signs, neurological development, and overall well-being.
Pain Management: Preterm babies often undergo various medical procedures, which can cause discomfort. NICUs focus on minimizing pain through gentle handling, pain medications, and other strategies.
Family-Centered Care: NICUs recognize the importance of family involvement. Parents are encouraged to participate in their baby’s care, including skin-to-skin contact (kangaroo care), bonding, and breastfeeding support.
Neurodevelopmental Care: The Newborn Individualized Developmental Care and Assessment Program (NIDCAP) aims to reduce stress associated with NICU care. It focuses on controlling external stimuli (light, noise) and providing individualized care
